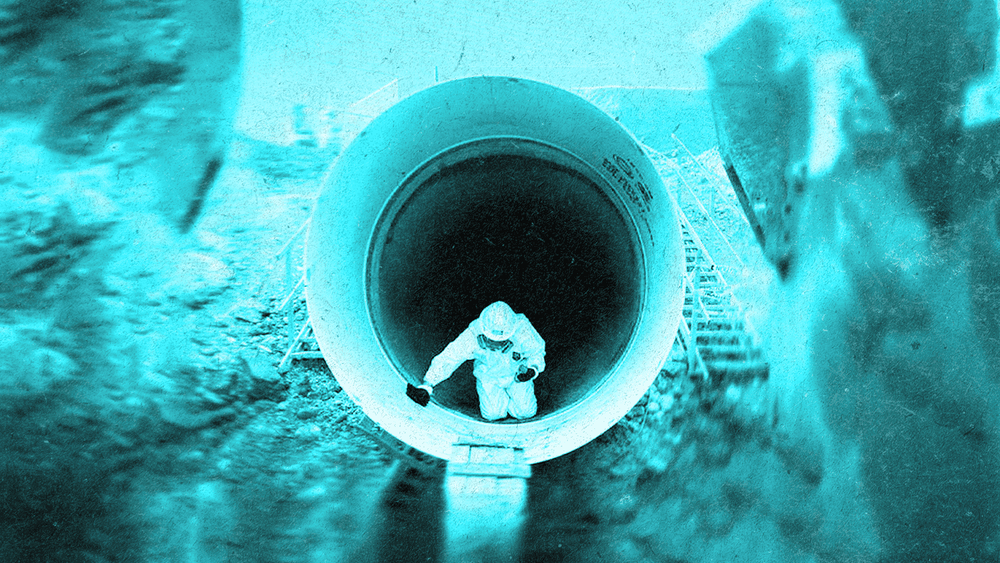
The Alpha House DOAP team checks in on a homeless Calgarian in December. Photo: Todd Korol
Calgary shelters brace for coronavirus
It’s time to treat housing as health care. Immediately.
Over the weekend, as temperatures dropped to -25 and most residents of Calgary hunkered down in their homes, local shelters were packed with the city’s most vulnerable.
At Alpha House, 105 people slept on mats, lined up in rows on the floor, barely a limb-length apart. Another 15 clients were relocated to different shelters around the city. Though Alpha House can house up to 120 people, its staff is trying to place as much space as possible between bodies right now.
They’ve asked clients to sleep head to toe, a configuration that increases distance between faces. A sign went up recently on the front door to inform anyone coming into the shelter that they must have their hands sprayed with disinfectant upon entry.
COVID-19 has not arrived here yet. But health care workers and staff, who keep their ears alert for any coughs, fear it is only a matter of time before the virus moves through this population with speed and ferocity.
We need a measure of mercy from our public officials to make sure there are more alternative places where people can go.
“When the community transmission of this virus starts, this is the high-risk situation,” said Dr. Bonnie Larson, a family physician with CUPS.
“We need space, stuff, systems and staff just like everybody else, just like the general response—but we're starting at baseline.”
Protection unequal as pandemic sets in
COVID-19 selects without socioeconomic discrimination. But the tools for protection are not equally distributed.
People who rely on crowded shelters for housing cannot physically isolate, especially in frigid temperatures. They do not have easy access to water and soap, hand sanitizer or wipes.
The effects of COVID-19 in Calgary will be made worse because of a slow response to the province’s homeless, Larson says.
“There are still so many uncertainties but we know for sure that our population is going to be hit very hard,” she said.
There are still so many uncertainties but we know for sure that our population is going to be hit very hard.
According to figures from the Calgary Homeless Foundation, 2,911 people were experiencing homelessness in Calgary in 2018.
Homeless Calgarians are twice as vulnerable because they have many of the conditions associated with worse health outcomes: chronic obstructive pulmonary disease, diabetes, liver failure, substance use disorders and mental health issues.
Also, they are often “chronologically older” than their age would suggest, says Larson. In this population, someone who is 40 may have the expected health of someone closer to 70. Their symptoms can go unnoticed in the shelter system, she says.
On most days, coughs and moans are part of the regular undertone in the shelter.
Homeless Calgarians need places to isolate
I spent part of the last two weeks learning about CAMPP, Calgary’s mobile palliative care program for the homeless. I followed nurses Dan Grover and Troy Speechly into shelters and supportive housing units.
Grover once described the job as looking for people who’ve fallen into cracks in our health care system.
Last week, when I saw Grover at Alpha House, we talked about COVID-19, and the sudden urgency that has set in across the city. He raised his hands, indicating the space around him, and said, “So much of what we were talking about, so much of our stresses would be completely alleviated if we just saw housing as health care.”
So much of our stresses would be completely alleviated if we just saw housing as health care.
Right now, no large-scale plan exists for helping Calgary’s homeless through the pandemic. There are no isolation units, no specific strategies for testing and no guidelines on what to do for this population.
The employees who work at shelters are not medical professionals, and there’s a high turnover of staff due to chronic under-funding and high stress levels, says Dr. Jeannette Waegemakers Schiff, a professor of social work at the University of Calgary.
Waegemakers Schiff was part of a team of Canadian researchers who put together a plan for pandemics and homelessness after H1N1.
Shelters should not run at full capacity during a pandemic, she says.
“We need a measure of mercy from our public officials to reach out and make sure that there are more alternative places where people can go to stay warm and to stay safe, and to not be so crowded together with each other.”
AHS is working on a guideline for the Alberta’s homeless, which should be available in the next few days, Dr. Deena Hinshaw, Alberta’s chief medical officer of health, said during a press conference on Monday.
All that we’re doing is scrambling around watching the frontline just disappear.
But Larson says Calgary’s homeless need more than guidelines—and quickly.
“All that we're doing is scrambling around watching the frontline just disappear.”
Larson called on the city and province to provide extra funding specifically for care of the homeless. She wants isolation units for the homeless—places where they can go when they first have symptoms, are waiting for test results or have been released from hospital.
Larson doesn’t want to wait for people to show up in the shelter system with symptoms before they are tested. She feels a better option would be active surveillance in the community.
Otherwise, cases will go unrecognized and risk further spread into the community.
A need for empathy, too
Ty Eggenberger, the acting manager of the AHS community paramedic service, says different efforts are necessary for the homeless in order to achieve the same level of care as everyone else in Alberta.
If people in Calgary want to help, they can begin with a basic understanding that some people's circumstances are different, and different circumstances need additional services to achieve the same level of care.
“We're very good about understanding when we have a special circumstance for ourselves or for our loved ones,” he said, “but sometimes we lose sight of that when we don't understand people's circumstances.”
The homeless all live under the same rule: The general public is always more afraid of us than we are of them.
Dean, who did not want his last name published, is staying in one of the palliative beds on the medical unit at the Drop-In Centre, after being diagnosed with lung cancer in February. He’s supposed to move to supportive housing later this week, but now everything is up in the air. He coughs from his cancer and that might be enough to keep him from housing right now.
He is well-aware of COVID-19 and the risks, but not afraid, he said. The homeless “live in a situation where coming across virulent problems is not uncommon.”
Calgary’s homeless aren’t desperate for physical distance and social isolation because they’ve always been isolated, he says.
“You have to remember exactly how many people go out of their way to avoid the homeless. The homeless all live under the same rule: The general public is always more afraid of us than we are of them.”
Christina Frangou is a Calgary journalist who covers health and social issues. Her reporting has garnered multiple national awards and nominations, including a National Newspaper Award in long feature writing for a story about her experience as a young widow.
The Sprawl is crowdfunded, ad-free and made in Calgary. We rely on reader support—just a few dollars a month—to publish local stories like this one. You can help by signing up today as a Sprawl member. Thanks for supporting independent journalism!
Support independent Calgary journalism!
Sign Me Up!The Sprawl connects Calgarians with their city through in-depth, curiosity-driven journalism. But we can't do it alone. If you value our work, support The Sprawl so we can keep digging into municipal issues in Calgary!